How I learned to live with chronic illness—and chronic hope.
At age 22, just months after graduating from Puget Sound, Jennifer Cramer-Miller ’87 experienced a sudden, life-threatening disease—one that would lead to four kidney transplants over the next 20 years. In a book published this August, Cramer-Miller chronicles the uncertainty, her will to survive, and her determination to find joy. What follows is an excerpt from that book.

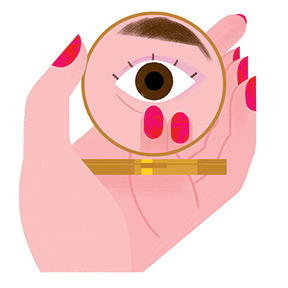
One morning at the tail end of my 22nd year, while I was downing coffee with my roommate, my face felt peculiar. Squishy. Leaning toward Lisa over the table in our apartment’s tiny kitchen, I said, “Check this out. Don’t my eyes look smaller?” “Too much salt?” Lisa asked, before blowing steam from the top of her mug.
“Maybe.” I pressed my fingers into the puffy skin that surrounded my upper and lower lashes.
It was Saturday, my energy lagged, and the warm cocoon of my duvet called. Eventually, I motivated myself to shower and throw on jeans and a chunky November-style sweater. Another glance in the mirror. Typically, I would blame a little puffiness on the regular suspects, PMS or MSG. But on this day, the skin around my eyes resembled spongy marshmallows.
I wondered if more coffee might help. It didn’t. My brain felt as dull as the Seattle sky outside the apartment windows, where falling raindrops played percussion on glass. Lisa took off to hawk hosiery during her Nordstrom shift downtown. I stayed in. As the hours ticked by, my legs felt tight, and my inner voice vacillated between calm dismissal (it’s nothing) and far-flung possibilities (bubonic plague?). I had no idea to what extent—but I was not okay.
Sprawled on the couch with the television on, I called my boyfriend, Nick, and vented about my dilemma.
“I’ll come over tonight with some booze to flush you out,” he offered, sounding lighthearted.
“Skip the booze. Just come over,” I said. “There’s no party potential tonight.”
Six months earlier, Lisa and I had graduated from Puget Sound. I met Nick in college too, but with more credits to complete, he still lived close to campus in Tacoma.
That night, after Lisa came home from work, Nick arrived with a bottle of wine. The three of us sank comfortably into the couch, but my mind was far from relaxed. My eyes seemed worse, the skin around my ankles felt taut, and I had no fitting reference for these symptoms.
“Drink up.” Nick handed me a glass filled to the brim.
“Jen, wine won’t do it. You need a doctor,” Lisa said firmly.
“I don’t have one.”
During college, the student health building was an easy walk across campus. But I hadn’t needed a doctor since graduation, and as a recent resident of Seattle, I knew nothing of the city’s medical clinics.
“Get one.”
The next day, I dialed my parents and explained that I felt off. “Maybe I’m coming down with the flu?” I said in a measured voice. I didn’t want to alarm them, but that didn’t work. Although their Minnesota home was miles from Washington, they jumped into action.
Monday morning, Dad reported he’d gotten a referral to a Seattle internist from his doctor in Minneapolis. They set an appointment for the next day, Tuesday, at 11:00. I noted it on my calendar and dashed out the door so I wouldn’t be late for work. I snagged the bus from our Capitol Hill apartment to my office in Pioneer Square, where I worked as a public relations intern.
Same routine as always. I raced into the building on Occidental Avenue, jogged through the lobby to catch the elevator, and stepped into the office on the sixth floor where everyone buzzed—20 or so professional bees in a frenzy of creative production. I sat at my designated intern cubicle and resumed updating a CEO database, trying to ignore my swollen eyes, feet, and fingers.

I was excited about this choice internship at Cole & Weber, a subsidiary of a national PR firm, Ogilvy & Mather. When my boss, Stacy, selected me from 200 applicants, I let out an involuntary squeal and shimmied a happy dance. With my foot in the door and my work in the mix, I planned to secure a future position. I wanted to put my newly earned business degree to work. So I intended to be the perfect intern.
That’s why I reluctantly approached Stacy to tell her I had a doctor’s appointment the next day and had to leave before my lunch break. She tried to scrutinize my face, but I lowered my head. Fine with me if she saw the same hard-to-tame, medium-length brunette hair and freckles splattered on my nose—but I didn’t want her to stare at the swelling surrounding my brown eyes. “Everything okay?” she asked. She was three years older, and our relationship was strictly professional. But at this moment, she seemed more concerned about me than my performance.
I forced a perky tone. “Oh, I think so. Just need to be sure.”
My daytime internship was for career advancement, but the pay wasn’t much. So at night I sold costume jewelry and taffeta prom dresses at a department store. Late ’80s fashion was ripe with Lady Diana-inspired shoulder pads, vivid colors, and lots of chunky costume jewelry to complete the look. Pushing accessories and special-occasion dresses covered the extra money I needed to pay my rent. That night, as I exchanged pleasantries and sold boatloads of gold necklaces and silver earrings, I couldn’t ignore the discomfort that pressed against my skin.
On Tuesday, I drove to the University District to explain my symptoms to a doctor. A nurse drew my blood and asked me to pee in a cup. Then I waited alone in an uncomfortable wooden chair propped against the wall and focused on the vinyl wallpaper and tiles—a study in beige on beige. Windowless clinic rooms are never cheerful, but thankfully in my young life, I hadn’t seen many. The doctor walked in and sat down at the little desk next to me.
He was tall and thin, with brown leather shoes that he undoubtedly chose for comfort over style. His face looked serious—no smile or friendly eye twinkle—and his white hair matched his white doctor’s coat. He delivered his words softly, but they hit hard. “I’m sorry, young lady. The result indicates your kidneys are damaged.”
I gave him a few seconds to tell me it was a joke, but he didn’t seem like the jokester type, and come to think of it, how unfunny of a joke would that be? My mind raced with nonsensical thoughts. Yet this doctor was no-nonsense (his practical shoes … case in point), and this situation was the farthest thing possible from a joke.